PerioQuest
PerioQuest is a self-assessment test for predisposition to periodontitis for the general population, providing information about it, along with a vídeo demonstrating how to examine the mobility of our teeth.
The PerioQuest test was developed using information from the PerioProject data-base, a predictive model of tooth loss for dental professionals designed to determine periodontal prognosis, predicting what will happen to the teeth of people who have received treatment and come in for a check-up.
What does it mean Perioquest to general population?
The information provided by Perioquest provides the answer to what many patients want to know: whether they are going to lose their teeth.
The traditional way of making a professional prognosis was based on indices to establish various prognosis categories: good, guarded, poor, etc., but its accuracy was quite limited. The guarded prognosis essentially stated that a tooth might be lost or not, without specifying further. In contrast to this category with little meaning, Perioquest's prediction specifies which teeth might be lost and approximately when, achieving a high percentage of accuracy (81.4%). Based on this information, it is possible to make the most accurate decision in each case.
Perioquest represents an objective and reliable alternative for making decisions of enormous relevance, such as extracting all teeth to replace them with implants. Faced with this crucial step, it is logical to have an objective and reliable tool to incorporate alongside the professional's judgment, often limited to personal experience or a preference for a specific treatment.
Periodontal disease
Periodontal disease is one of the most common chronic diseases in humans. The bacteria that accumulate on the gums initially cause a superficial inflammation called gingivitis. If the bacteria penetrate deep below the sulcus, the inflammatory process progressively destroys the tissues that hold the teeth in place. Without treatment, this will ultimately result in tooth loss.

The edge of a healthy gum adapts perfectly to the shape of the tooth, leaving a triangular space between the teeth (the interdental papilla)

The margin of the gum is slightly separated from the tooth by one or two millimeters, forming the gingival sulcus. Its depth is measured by inserting a periodontal probe. Daily brushing should eliminate the bacteria that accumulate in the sulcus.
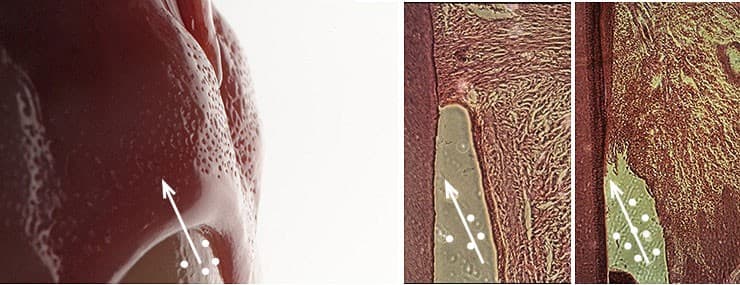
If the bacteria penetrate the sulcus, the internal epithelium of the gums is destroyed and the disease gradually destroys the tissue that holds the tooth in place.
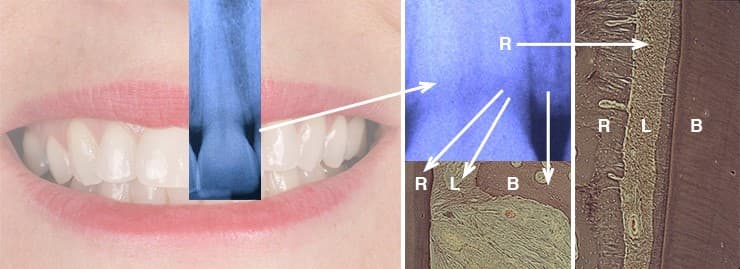
The tissue that supports the tooth is made up of the periodontium, which includes the gums, the tooth root surface (R), the alveolar bone, where the root is embedded (B), and the ligament that joins the root to the bone (L)
Manifestations
There are only a few signs of periodontal disease at the outset, including bleeding gums and inflammation. The gums may increase in volume or partially disappear, exposing the root (gingival recession). Sensitivity is also common, as is the appearance of gaps as the gums between the teeth (interdental papilla) recede, even producing separations between the teeth.
At the start of the disease, the gingival sulcus between the tooth and the gum deepens, forming the periodontal pocket, the depth of which can be measured with a probe. The gums can swell when inflamed or even disappear (gingival recession), especially if they are thin. As seen in these two examples of mild periodontitis, it is common for areas of swollen gums and gingival recession to coincide.

Diagnosis
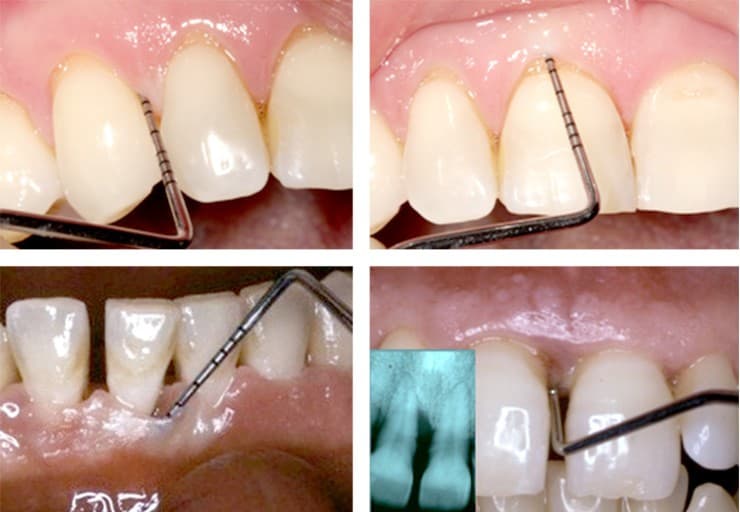
Early diagnosis of the disease is extremely important, as there are few symptoms and these might go unnoticed. Once tooth mobility becomes apparent, the disease has usually reached an advanced stage. The diagnosis is performed by measuring loss of the tissue that holds the teeth in place. Supporting bone loss is measured by x-ray. Gum loss is assessed by means of periodontal probing, which measures the amount of gum that has been lost (gingival recession) and in particular the amount of loose gum (periodontal pocket). Other diagnostic parameters are bleeding gums, tooth mobility and tests to identify the type of bacteria present.
In the photos, the probe confirms that there is a 2 mm sulcus, but no periodontal pocket. In the bottom left photo, a pocket is beginning to form. The following photo shows a very deep pocket, coinciding with significant loss of the bone holding the tooth in place.
Treatment
Basic treatment is administered inside this periodontal pocket and consists of eliminating the bacteria and tartar adhered to the root surface. This is performed with small, sharp instruments (for root scaling and planing) that fit inside the periodontal pocket, since the gum is separated from the tooth. There are complementary alternatives, such as surgery to ensure that the deepest pockets are clean, to reduce pocket depth and to regenerate lost tissue.
Long-term success requires regular periodontal maintenance check-ups every 3 to 6 months, depending on the severity and predisposition. These can then be scheduled once every 12 months if long-term stability is confirmed. This check-up consists of re-measuring the pockets and inflammation and eliminating any bacteria that may have gotten inside, before additional damage occurs.
Periodontal prognosis
Knowledge of the periodontal prognosis or future of the affected teeth is extremely important for the professional, and especially for the patient. This is the idea behind PerioProject , which was created so dental professionals can determine the prognosis for teeth that have been or will be treated for periodontal disease. This predictive model calculates the probability of losing each tooth, making it possible to set expectations for dental survival, i.e., how long the affected teeth can last.
This information provides the professional with an objective, reliable tool that will help him or her to select the best treatment plan. One good example is the decision to extract all of the teeth and replace them with implants in the most advanced cases. Such an important decision should be based on the best possible knowledge regarding the prognosis. It is reassuring for the patient to know that the prognosis is good.
Periodontal prognosis is usually good in the long term for most patients. Only a small percentage of patients that receive maintenance check-ups suffer a poor outcome and lose more teeth. This often occurs in association with negative factors, such as the disease being at a highly advanced stage, tobacco use, grinding of the teeth (bruxism), etc.
Self-test
Can I find out whether I have periodontal disease and what chance there is of me losing my teeth? Although only professionals can provide a valid, definitive diagnosis, it is possible to find out the tendency of your disease and estimate the risk of losing teeth in the future.
The PerioQuest self-test is very simple and can provide extremely valuable information. Check the boxes as accurately as possible and the program will estimate the need or urgency for a professional diagnosis and prognosis.
Self-test

Tooth mobility
The test to detect tooth mobility is especially important. The video tutorial to examine tooth mobility explains how this is done with the help of another person and using two chopsticks. Your assessment might be much more reliable than you think.
Watch videoThe most frequently used method for finding out whether a tooth moves is actually the least reliable: putting your fingers in your mouth, grasping the tooth and trying to move it. The correct method is shown in the video.
Assessment
Category 0: Teeth can have minimal, almost imperceptible mobility.
Category 1: If the tooth moves by about one millimeter.
Category 2: If it moves between one and two millimeters.
Category 3: If it moves more than that, or can even be pressed into the gum.
If you detect even the slightest movement, see your dentist.
Categories 2 and 3 may reflect the presence of a serious disease.
